Why does sleep paralysis happen? This question has plagued countless individuals who have experienced the terrifying sensation of being conscious but unable to move. Join us as we delve into the depths of this enigmatic phenomenon, exploring its causes, triggers, and management strategies.
Brace yourself for a spine-tingling journey into the realm of sleep’s dark side.
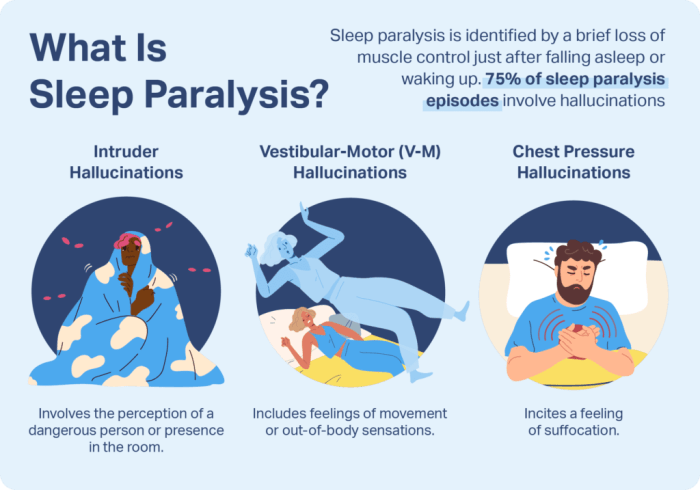
Sleep paralysis is a temporary inability to move or speak that occurs while falling asleep or waking up. It is often accompanied by vivid hallucinations, creating a surreal and often frightening experience. While it can be a distressing occurrence, understanding the underlying mechanisms can help alleviate anxiety and empower individuals to manage their episodes effectively.
Pathophysiology of Sleep Paralysis

Sleep paralysis is a temporary inability to move or speak that occurs while falling asleep or waking up. It is caused by a temporary disruption in the brain’s normal sleep-wake cycle.
During normal sleep, the brain produces a chemical called gamma-aminobutyric acid (GABA), which inhibits muscle movement. This prevents us from acting out our dreams. When we wake up, GABA levels decrease and muscle movement is restored.
In people with sleep paralysis, GABA levels do not decrease as quickly as they should. This can lead to a temporary paralysis that can last for a few seconds or minutes.
Brainwave Activity and Muscle Atonia
Sleep paralysis is associated with a specific pattern of brainwave activity. During sleep paralysis, the brain produces high-frequency brainwaves called beta waves. These brainwaves are typically associated with wakefulness.
The presence of beta waves during sleep paralysis suggests that the brain is not fully awake. This can lead to a state of confusion and disorientation.
Hormonal and Neurotransmitter Imbalances
Sleep paralysis may also be caused by hormonal and neurotransmitter imbalances. For example, people with low levels of the hormone serotonin are more likely to experience sleep paralysis.
Serotonin is a neurotransmitter that is involved in mood regulation and sleep. Low levels of serotonin can lead to insomnia and other sleep disorders.
Triggers and Risk Factors: Why Does Sleep Paralysis Happen
Sleep paralysis is often triggered by external factors that disrupt the normal sleep-wake cycle. These triggers can include:
- Stress:Emotional distress and anxiety can interfere with sleep patterns, making individuals more susceptible to sleep paralysis.
- Sleep deprivation:Insufficient sleep can disrupt the body’s natural sleep-wake rhythm, increasing the likelihood of experiencing sleep paralysis.
- Irregular sleep schedules:Frequent changes in sleep patterns, such as working night shifts or staying up late on weekends, can confuse the body’s internal clock and increase the risk of sleep paralysis.
Certain medical conditions and external factors can also increase the risk of sleep paralysis:
Medical Conditions, Why does sleep paralysis happen
- Narcolepsy:A neurological disorder characterized by excessive daytime sleepiness, narcolepsy is strongly associated with sleep paralysis.
- REM sleep behavior disorder:A condition where individuals physically act out their dreams, REM sleep behavior disorder can lead to sleep paralysis when the brain is still in REM sleep but the body has awakened.
Medications and Substance Use
- Antidepressants:Certain antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), have been linked to an increased risk of sleep paralysis.
- Alcohol and drugs:Alcohol and recreational drug use can disrupt sleep patterns and increase the likelihood of sleep paralysis.
Subjective Experiences and Hallucinations

Sleep paralysis is a state of temporary immobility that occurs while falling asleep or waking up. During this state, individuals are aware of their surroundings but are unable to move or speak. The experience can be accompanied by a range of subjective experiences and hallucinations that can be both frightening and confusing.
Emotional Impact
The emotional impact of sleep paralysis can be significant. The inability to move or speak can trigger feelings of fear, anxiety, and panic. Some individuals may experience a sense of suffocation or pressure on their chest, which can further intensify the feelings of distress.
Auditory and Visual Hallucinations
In addition to emotional distress, sleep paralysis can also be accompanied by auditory or visual hallucinations. These hallucinations can range from simple sounds, such as buzzing or ringing, to complex visions, such as seeing figures or animals in the room.
The content of the hallucinations can vary widely and may be influenced by cultural and personal beliefs.
Cultural and Historical Interpretations
Sleep paralysis has been interpreted in different ways throughout history and across cultures. In some cultures, it is seen as a supernatural experience, attributed to spirits or demons. In other cultures, it is believed to be a medical condition or a sign of mental illness.
Despite the varying interpretations, sleep paralysis remains a common experience that can have a significant impact on individuals. Understanding the subjective experiences and hallucinations associated with sleep paralysis can help to reduce the fear and anxiety that it can cause.
Management and Prevention Strategies
Managing and preventing sleep paralysis involves a multifaceted approach encompassing lifestyle modifications, relaxation techniques, and cognitive-behavioral therapy. Additionally, sleep hygiene and regulation play a crucial role in reducing the frequency and severity of episodes.
Sleep paralysis occurs when the brain awakens from REM sleep while the body remains in a state of temporary immobility. This can be a frightening experience, but it is usually harmless. Some researchers believe that sleep paralysis may be related to the phenomenon of “septets,” or groups of seven notes that are often used in music.
What is a septet ? A septet is a group of seven musicians or singers, or a piece of music written for seven voices or instruments. The term can also refer to a group of seven things, such as the seven days of the week or the seven deadly sins.
While the connection between sleep paralysis and septets is not fully understood, it is an intriguing possibility that suggests that there may be a deeper connection between our sleep and our musical experiences.
Lifestyle Modifications
- Establishing a regular sleep schedule, even on weekends, ensures consistency in the body’s natural sleep-wake cycle.
- Creating a conducive sleep environment involves optimizing bedroom temperature, darkness, and noise levels for restful sleep.
- Avoiding caffeine and alcohol before bedtime prevents disruptions in sleep patterns and reduces the likelihood of sleep paralysis.
- Engaging in regular exercise promotes overall well-being and can improve sleep quality, but it’s important to avoid exercising too close to bedtime.
Relaxation Techniques
- Deep breathing exercises, meditation, and yoga promote relaxation and reduce stress levels, which can contribute to sleep paralysis.
- Progressive muscle relaxation involves tensing and releasing different muscle groups to alleviate tension and induce relaxation.
- Visualization techniques, such as imagining a peaceful scene or counting backward, can help calm the mind and prepare the body for sleep.
Cognitive-Behavioral Therapy (CBT)
CBT is a form of psychotherapy that addresses the underlying thoughts and behaviors associated with sleep paralysis. It involves:
- Cognitive restructuring to challenge and modify negative beliefs about sleep paralysis, reducing anxiety and fear.
- Exposure therapy to gradually confront and overcome the fear associated with sleep paralysis, increasing confidence and control.
- Relaxation techniques to manage stress and anxiety, improving overall sleep quality.
Medications and Other Interventions
In severe cases, medications such as antidepressants or benzodiazepines may be prescribed to reduce anxiety and improve sleep quality. However, it’s essential to consult a healthcare professional before using any medications.
Other interventions include:
- Sleep deprivation therapy involves deliberately restricting sleep to induce a “rebound” effect, potentially reducing sleep paralysis episodes.
- Transcranial magnetic stimulation (TMS) is a non-invasive procedure that uses magnetic pulses to stimulate specific areas of the brain, potentially reducing sleep paralysis.
Differential Diagnosis and Treatment
Sleep paralysis can share similar symptoms with other conditions, making differential diagnosis crucial to rule out underlying medical conditions and ensure appropriate treatment.
Conditions that mimic sleep paralysis include seizures, transient ischemic attacks (TIAs), and psychiatric disorders such as narcolepsy and cataplexy. Seizures can cause temporary loss of consciousness and involuntary movements, while TIAs can lead to sudden weakness or numbness on one side of the body.
Psychiatric disorders may involve episodes of muscle weakness or paralysis that resemble sleep paralysis.
Medical Treatment
Medical treatment for conditions mimicking sleep paralysis depends on the underlying cause. Seizures may require anticonvulsant medications, TIAs may necessitate blood thinners or lifestyle changes, and psychiatric disorders may involve psychotherapy or medications.
Psychological Treatment
Psychological treatments for conditions mimicking sleep paralysis focus on addressing the underlying psychological factors that contribute to the symptoms. This may involve cognitive-behavioral therapy (CBT) to challenge negative thoughts and behaviors, or exposure therapy to gradually reduce the fear associated with the symptoms.
Last Point
Unveiling the secrets of sleep paralysis has shed light on its complex interplay of neurological, physiological, and psychological factors. By recognizing the triggers and implementing preventative measures, individuals can reduce the frequency and severity of episodes. Moreover, seeking professional guidance can provide tailored management strategies, ensuring a restful and undisturbed slumber.